This post may contain affiliate links. Read our disclosure policy.
Polycystic ovarian syndrome (PCOS) isn’t a one size fits all diagnosis. There are different types of PCOS and each person can experience symptoms on a spectrum. Here we’re breaking down the different types, how to determine which one you have, and the best route for healing for each.

Table of Contents
- FAQs about PCOS
- How do I know if I have PCOS?
- How can I reverse PCOS naturally?
- The best resource for PCOS:
- General Labs for PCOS:
- Here are the Types of PCOS:
- Insulin Resistant PCOS
- Post-pill PCOS
- Inflammatory PCOS
- Adrenal PCOS
- Other causes of PCOS
- General PCOS treatments that will help with any type of PCOS
- More of Molly’s posts about PCOS:
This is a guest post written by my functional CNP Julie Grafmeyer from CAPS Wellness Center. I’ve been working with her for years and she helped me reverse my PCOS symptoms. She’s worked with so many clients with PCOS and has a wealth of knowledge about it and I can’t wait to share this information with you!
FAQs about PCOS
How do I know if I have PCOS?
PCOS is a group of symptoms caused by an imbalance in hormones. The primary diagnostic criteria according to the Androgen Excess Society Criteria and the Rotterdam Criteria include:
- Irregular periods and/or polycystic ovaries on ultrasound
- Signs (laboratory findings) or symptoms (such as acne or hirsutism) of high androgens
- And an absence of other causes of these symptoms.
How can I reverse PCOS naturally?
Once the diagnosis of PCOS has been determined, treatments including lifestyle modifications, supplements, and prescriptions, when necessary, help your body heal and find balance.
In order to be successful with your treatment plan, focusing on the individual drivers or triggers for your unique PCOS is imperative. Your individual story can include more than 1 trigger, and even more than 1 hormonal disorder.
I always recommend looking for the root cause of your symptoms. Start with the most obvious triggers, slowly peel back the layers, observe, listen, and learn from all the signals your body is sending you.
The best resource for PCOS:
My favorite PCOS reference is The Period Repair Manual by Lara Briden, ND. Please use this amazing resource to help determine which type of PCOS you may have and possible treatment options to target your triggers.
General Labs for PCOS:
There are many different lab tests that help differentiate types of PCOS. Remember, lab tests are not required for the diagnosis of PCOS, and every person’s lab results and presentation is unique. Many people also have more than 1 trigger. You might have insulin resistance, inflammation issues, thyroid disease, and vitamin deficiencies!
Typical early screening lab work to evaluate for the diagnosis of PCOS include the following:
- FSH
- LH
- Prolactin
- Estradiol
- Total and free testosterone
- DHEA-Sulfate
- Fasting glucose and insulin
- Hemoglobin A1c
- TSH, Free T4, and Free T3
- Lipid panel
- High sensitivity CRP
Your unique presentation, symptoms, and story will often lead your provider to order even more in depth testing. All of these things come together to help determine which type of PCOS you primarily are dealing with. Check out more about Molly’s blood work here.
Here are the Types of PCOS:
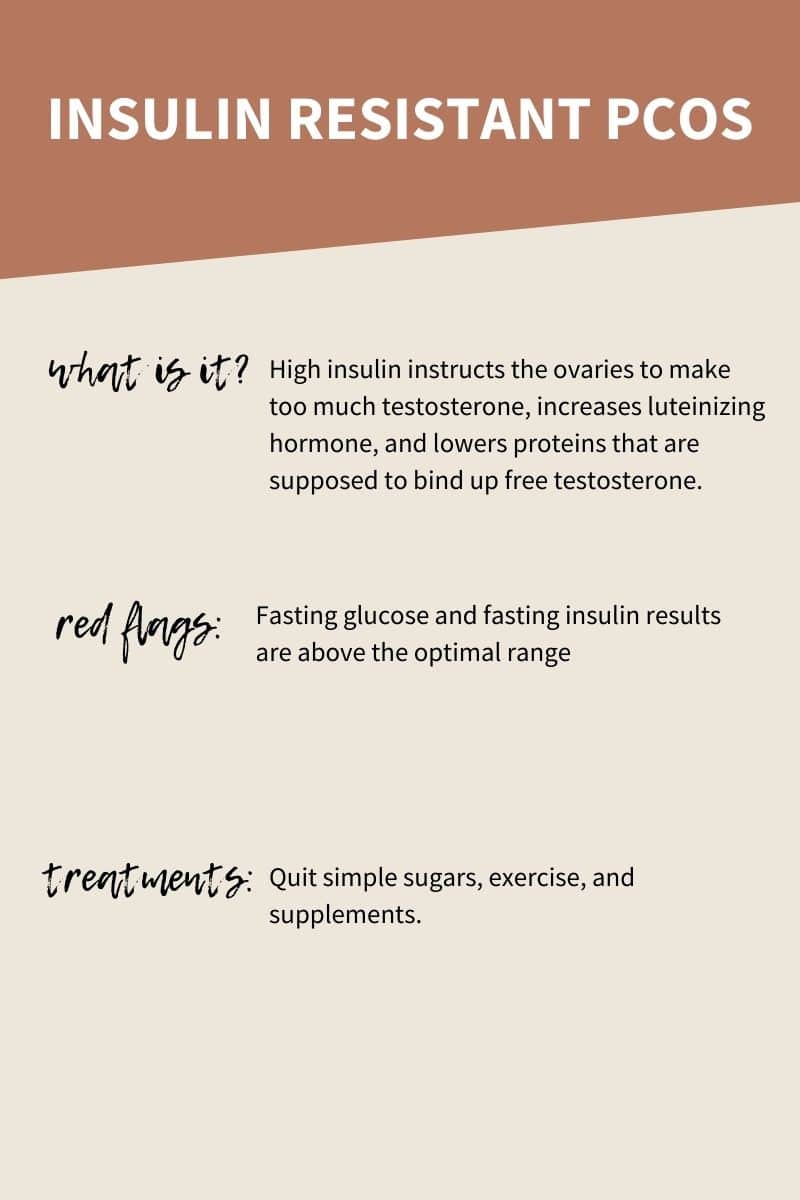
Insulin Resistant PCOS
What is Insulin resistant PCOS?
Insulin resistance is the most common trigger for PCOS. High insulin instructs the ovaries to make too much testosterone, increases luteinizing hormone (which increases testosterone), and lowers proteins that are supposed to bind up free testosterone (which increases active testosterone in your body).
One issue with insulin leads to at least three causes of high androgens. This is such a perfect example of root cause medicine. Focusing on treating the insulin.
Red flag test results:
- Fasting glucose and fasting insulin results are above the optimal range. Ideally, your fasting glucose should be less than 90 mg/dl and your fasting insulin should be less than 6.0 uIU/ml. It is important to remember that “normal” lab reference ranges don’t always mean optimal ranges. To control PCOS symptoms, these numbers often need to be optimal, not just normal.
Treatments for Insulin resistant PCOS:
- Quitting simple sugars and minimizing carbs, even trying intermittent fasting or the ketogenic diet if it is appropriate for you, are some of the most powerful ways to lower your blood sugar and insulin. Here are some great low carb recipes.
- Exercising and moving throughout the day allows your body to burn sugar and build muscle (which also burns sugar).
- Be sure to prioritize sleep and stress management. A lack of sleep and excess stress that isn’t managed will both lead to increased blood sugar.
- Supplements or prescriptions if necessary can be very helpful to help make you more insulin sensitive, lowering both your blood sugar and insulin.
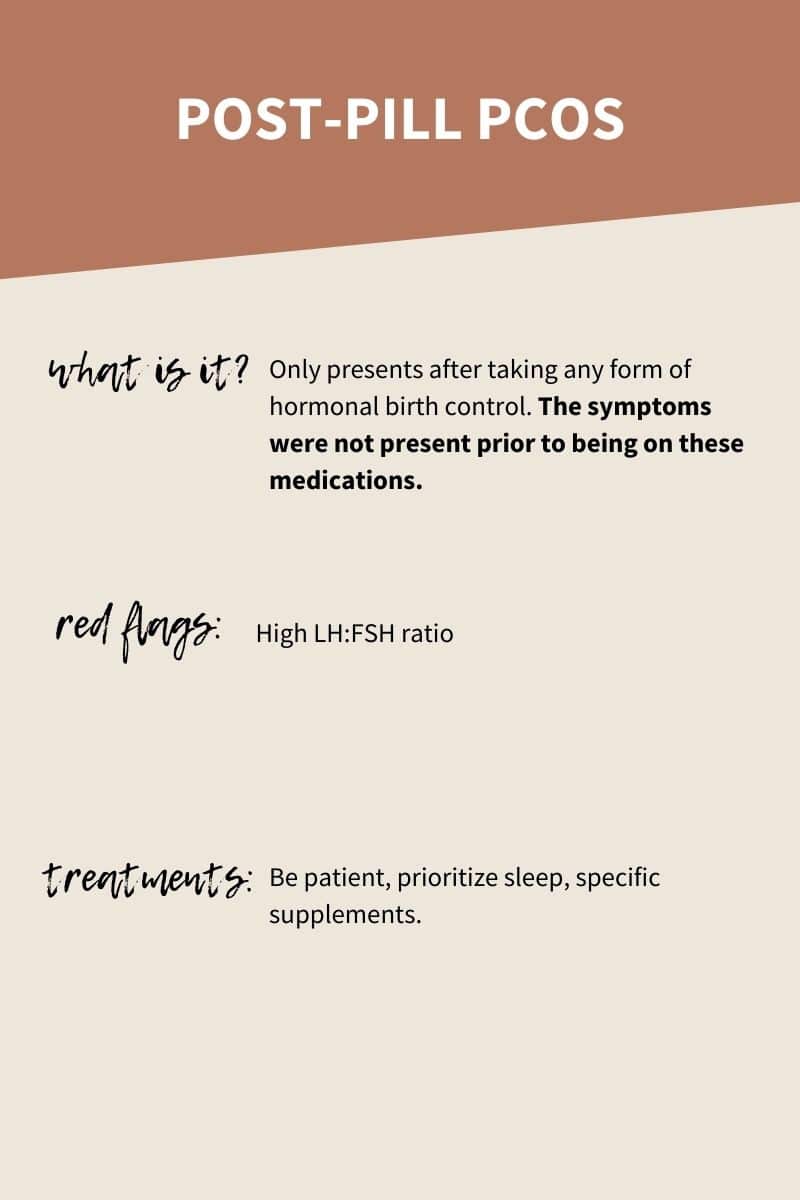
Post-pill PCOS
What is post-pill PCOS?
Post-pill PCOS only presents after taking any form of hormonal birth control. The symptoms were not present prior to being on these medications. If you went on HBC because of symptoms and irregularities and experienced them after coming off, you may want to look into the other types of PCOS.
What does the pill do to your hormones?
These medicines suppress ovulation so that you don’t get pregnant and some women will experience an increase in androgen production temporarily after stopping birth control, which causes symptoms such as acne, hair growth on the body, or hair loss on the head.
Hormonal contraceptives can cause or worsen insulin resistance. In some women these hormonal changes persist after stopping the contraception, causing symptoms consistent with PCOS. Beyond the Pill is a great resource to learn what HBC does to your body.
Red flag test results for Post-Pill PCOS
- Fasting glucose and fasting insulin results are well within the normal range
- Inflammation markers and symptoms are relatively normal
- High LH:FSH ratio
Treatments for post-pill PCOS
- Be patient
- Prioritize sleep, stress management
- Consider other specific supplements as directed by your healthcare provider to help lower androgens
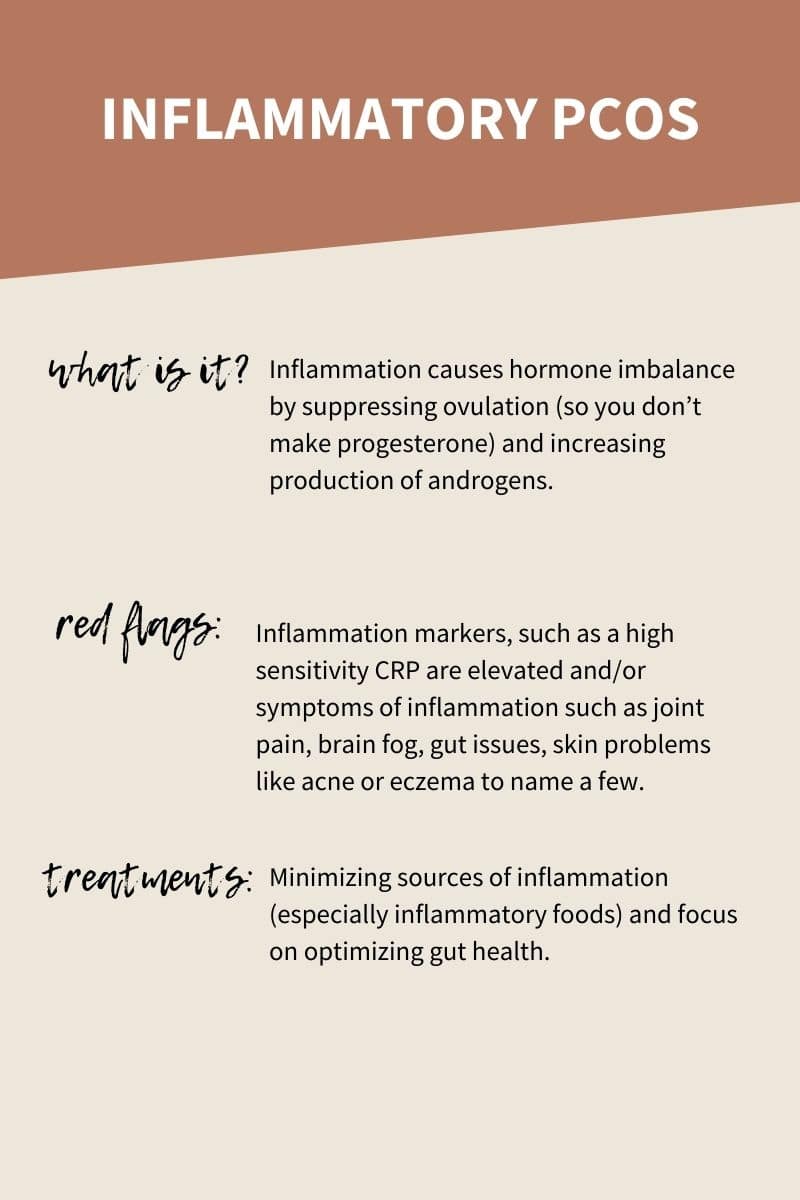
Inflammatory PCOS
What is inflammatory PCOS?
Inflammation causes hormone imbalance by suppressing ovulation (so you don’t make progesterone) and increasing production of androgens.
Inflammation directly decreases progesterone and increases androgens, and inflammation causes higher blood sugar and insulin, which causes higher androgens and decreased progesterone production.
Red flag test results
- Fasting glucose and fasting insulin results are within the normal range, but may not be perfect as inflammation can increase these numbers.
- Inflammation markers, such as a high sensitivity CRP are elevated
- And/or you have symptoms of inflammation such as joint pain, brain fog, gut issues, skin problems like acne or eczema to name a few.
Treatments for Inflammatory PCOS:
- Minimizing sources of inflammation, especially inflammatory foods or foods you have sensitivities to, is the first step. Always start your treatment by removing the triggers, then add supportive tools such as turmeric or omega 3 fatty acids to help your body heal and recover.
- Focus on optimizing gut health. Gut imbalances such as bacterial overgrowth, yeast overgrowth, chronic parasites, low digestive enzymes, and leaky gut are common sources of inflammation.
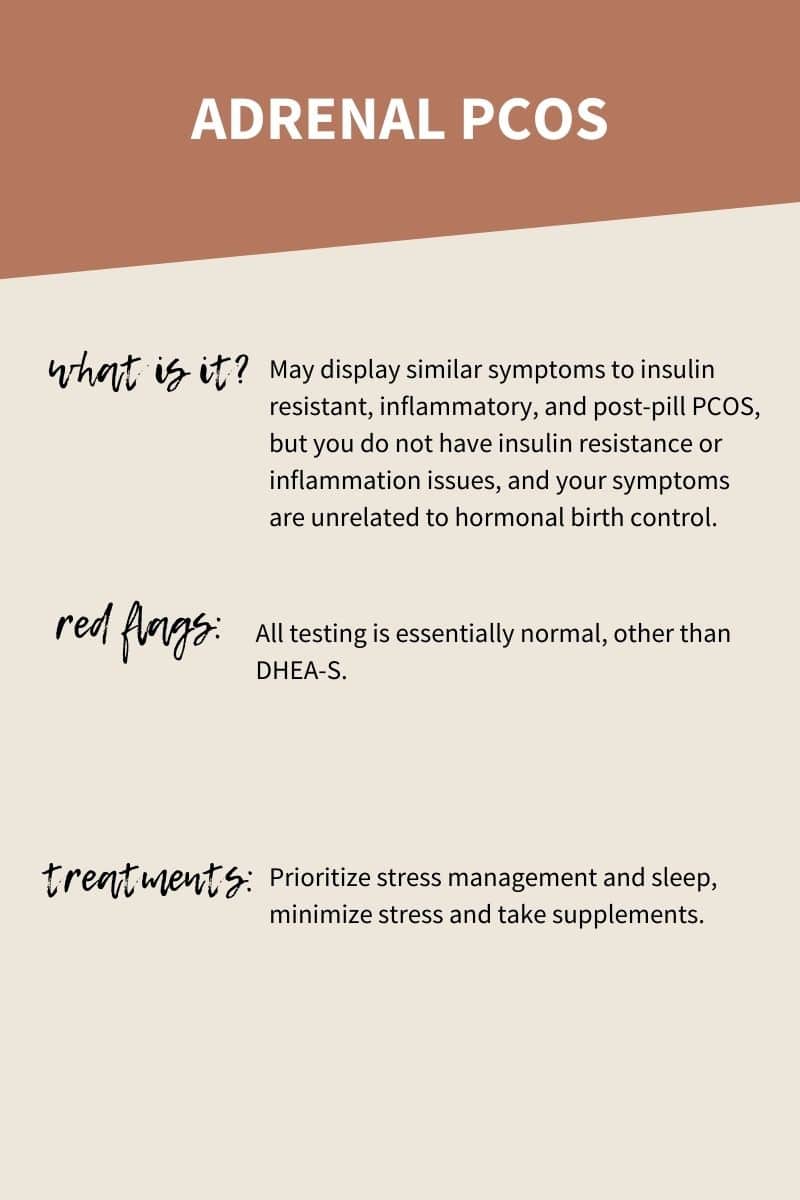
Adrenal PCOS
What is adrenal PCOS?
This type may display similar symptoms to insulin resistant, inflammatory, and post-pill PCOS, but you do not have insulin resistance or inflammation issues, and your symptoms are unrelated to hormonal birth control. The adrenal organs are responsible for controlling the stress response. When the stress response is not balanced, hormones are not balanced.
Red flag test results
- All testing is essentially normal, other than DHEA-S which is the androgen produced in the adrenal glands.
Treatments
- Prioritizing stress management by focusing on meditation, mindfulness, guided imagery or other stress management practices daily
- Prioritizing sleep
- Minimizing causes of stress including environmental toxins, over exercise, emotional triggers
- Supplements can be very helpful to help support the adrenal system and sleep
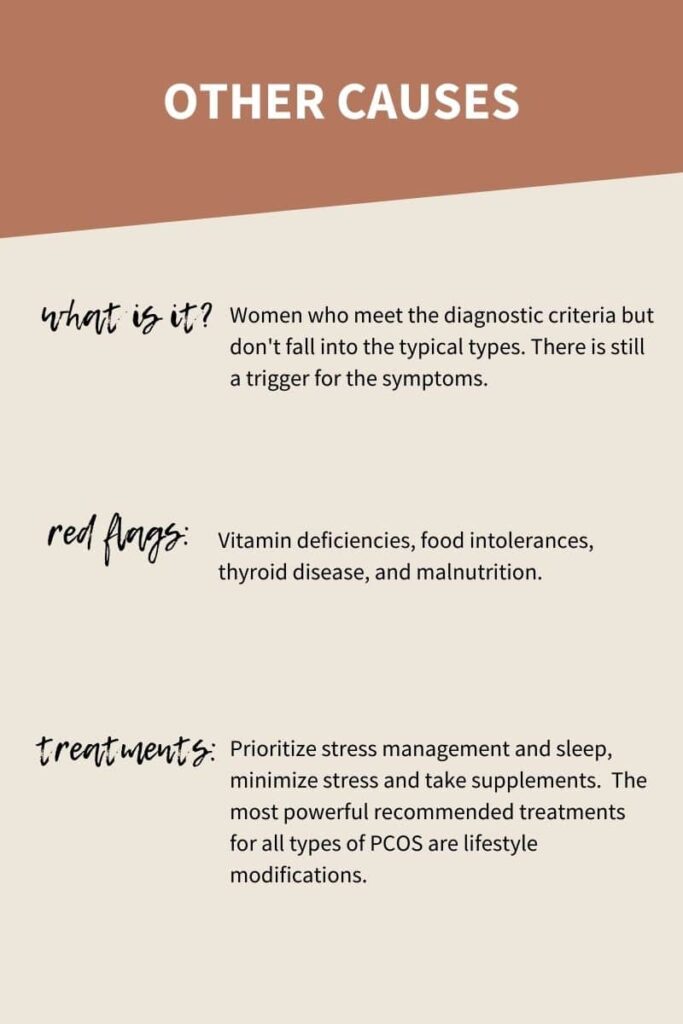
Other causes of PCOS
There are women who meet the diagnostic criteria for PCOS, but don’t have insulin resistance, inflammation or adrenal issues, and have not been affected by hormonal contraception. There is still a trigger for the symptoms, but it falls into this “other” category.
Vitamin deficiencies, food intolerances, thyroid disease, and malnutrition are a few examples of causes. There are also women whose trigger is never found, but the treatments, especially lifestyle modifications are still very powerful at controlling symptoms.
You are not alone.
Please remember, PCOS is a common hormonal disorder. You are not alone. The most powerful recommended treatments for all types of PCOS are lifestyle modifications. As you search for your trigger, start by working down this list, and as you go, listen and learn. You know you better than anyone else ever will. Use your intuition to guide your treatments, and seek medical advice along the way.
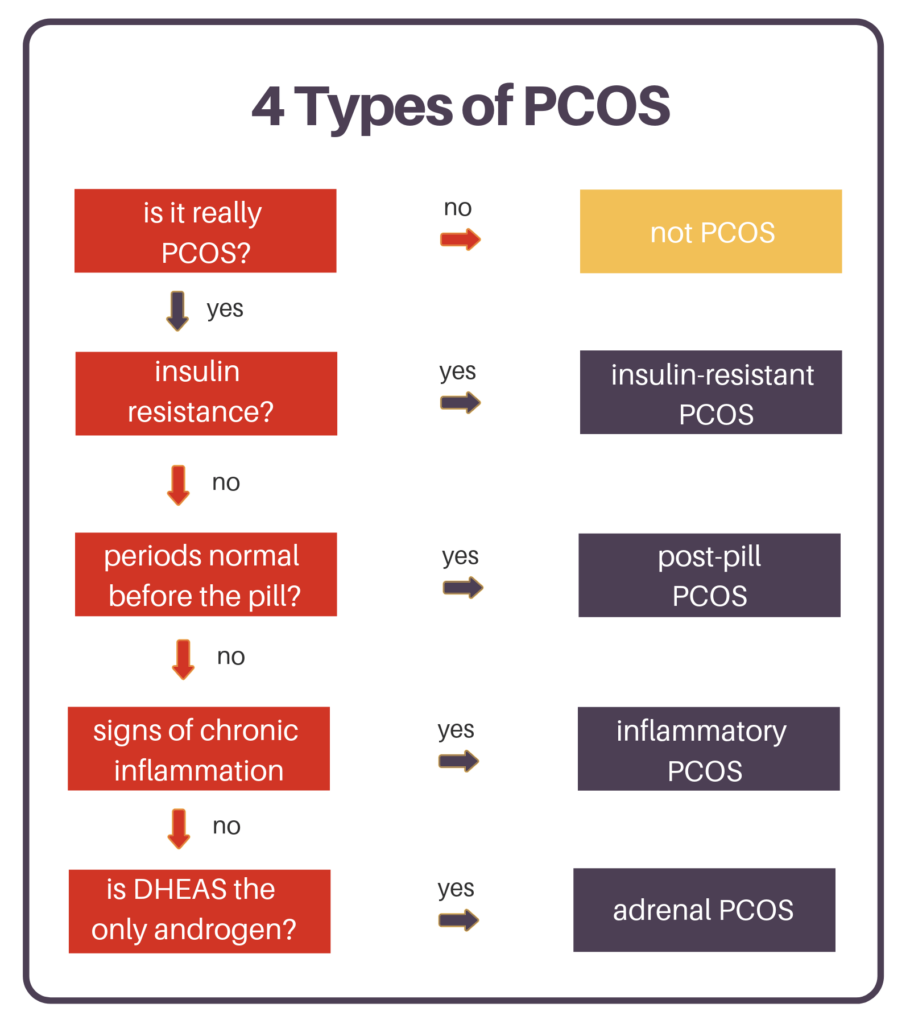
This flow chart was created by Dr. Lara Briden. She has a blog post about the types of PCOS as well and created this great graphic to explain how to narrow down which type you have.
General PCOS treatments that will help with any type of PCOS
- Minimizing processed and refined simple sugars.
- Minimizing inflammatory foods such as gluten and dairy. Learn more about an anti-inflammatory diet here.
- Optimizing your gut health to keep toxins out of your body, clear your old hormones, and keep inflammation low.
- Exercising regularly to burn sugar, build muscle, manage stress, and optimize sleep.
- Prioritizing a consistent daily stress management practice such as meditation, mindfulness, guided imagery, or any version of self-care that speaks to you.
- Sleep is a non-negotiable.
Here’s to happy hormones!


Hello, my name is shannon I’m a mom of two beautiful children 14.5 years apart, at 17 I was told I wouldn’t be able to have kids . Didn’t get diagnosed with pcos till 2012 two years after I got the marina placed. I had it taken out after five years of pain none of the dr I went to would take it out. In 2015 I finally found a Dr who would take it out, which should have been surgically removed, was ripped out. Which then caused me to bleed for four months straight. Found out that when I got pregnant with my son he connected where I was bleeding from.have my son may 2016 Pain continues, get gallbladder Removed 2017, pain still continues, hysterectomy 2018, verified PCOS endometriosis endometriosis pre-cancerous polyps on the cervix where the marina was positioned with this article is this proof that the marina is the cause of my health condition today the non-stop skin tabs constant plucking of the hair on the chin unmanageable weight. Mind you the pain still continues
Great article.. Helped me understand more about PCOS and most importantly, how that can be tackled. I also suffered from PCOS.I’m using lot of supplements like PCOS seeds, Healthveda.These supplements did not cure PCOS.Finally i found Solvve Supplement.Solvve supplement has helped me a lot to recover from PCOS.and I like that taste.It is like a juice.Now, I’m very happy and more healthy.Thank god!..I hope If you suffer from PCOS The below link will help you greatly.
https://www.solvve.in/
Hi Molly,
Thank you so much for this information. I am turning 40 next month. I would like to ask for your opinion. I was diagnosed last month with PCOS based on the slightly elevated DHEAS and stubborn acne on my chin area. I had a transvaginal ultrasound and showed that my ovaries have normal appearance and also states appearance consistent with polycystic ovaries. My period is regular and based on the type you shared, I am under Androgen and Inflammatory PCOS. I know I had been stressful emotionally and physically recently and my diet was not the best. My AMH level was 7.2 and this was the one that actually triggered me to request for a work-up from my OBGYN. I was suspicious that I might have PCOS. Based on the Ultrasound, I also had multiple fibroids but only one in the uterine cavity or endometrium.
My OBGYN prescribed Metformin 1500mg a day. Hysterectomy and myomectomy for my fibroid in the endometrium (1cm) since I still wanted to have a baby.
Is it ok to take the Metformin with my type of PCOS? We have a history of diabetes and there was a point that I also noticed that my fasting blood sugars were in the low 100s. It improved with diet modification though.
Is surgery a good option for my fibroid?
Thank you for your response and time. Appreciate it.
Hello, I was diagnosed with PCOS in March 2021, at least what my doctor said… I was on pill for two years, before pills I did not have any problems with my period, it was super regular. I stopped pills in September 2020, and I had no period for 3 months, then I had 14 day cycles, so I went to my doctor, who did my transvaginal ultrasound (polycystic ovaries) and said that I have PCOS. Only thing tested in lab was my progesterone, which was low. Then I asked her if it is possible, that I have pill induced PCOS, and she said there is no such thing… + Before going to my doctor (3 weeks before) I was urgently in hospital and another doctor performed transvaginal ultrasound, and my ovaries were normal. What should I do? I will see another doctor of course, but.. Thank you for your answer.
Hi Ana! I’m so sorry you’ve been going through all of this. Please know that there IS SUCH A THING as post pill PCOS. You can read more about it in Dr. Brighten’s book called, “Beyond the Pill.” She also has tons about it on her website: drbrighten.com. I highly recommend checking both out. So proud of you for advocating for yourself and not giving up. I know you’ll be able to balance everything and figure it out. If you haven’t checked out Parsley Health, they’re a great online option for functional medicine!